Page 7 - reflections_newsletter10
P. 7
REFLECTIONS
Dyslipidaemia
Dyslipidaemia Global Newsletter #10 2025
by 2040, and a 7.3% reduction by 2050, preventing 29 million deaths and 72 million non-fatal events. The population-based scenario
produced larger gains, with CVD events and deaths being reduced by up to 12% and preventing 51 million deaths and 130 million
non-fatal events over 2023–2050.
Dyslipidaemia
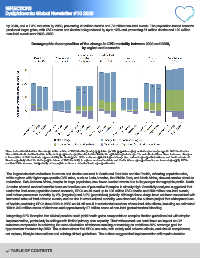
Demographic decomposition of the change in CVD mortality between 2020 and 2050,
by region and scenario
Three factors that determine the change in the number of CVD deaths (y-axis): population growth, population aging, and changes in age-specific CVD death rates.
The combined effect of the first two is the demographic change; the effect of the third is the epidemiological change. The net effect of these three factors on changes
in the number of CVD deaths is represented by the black points. SPCs enhance epidemiological change (i.e., reduced age-specific incidence and death rates) and
therefore partially offset the demographic drivers of CVD mortality. In regions such as East Asia and Pacific where age-specific rates are increasing rapidly, SPCs
could slow this increase, but probably not enough to achieve a net reduction in age-specific rates.
The largest absolute reductions in events and deaths occurred in South and East Asia and the Pacific, reflecting population size,
while regions with higher age-specific CVD rates, such as Latin America, the Middle East, and North Africa, showed smaller absolute
reductions. Sub-Saharan Africa, despite its large population, saw fewer averted events due to its younger demographic profile. North
America showed modest benefits because baseline use of preventive therapies is already high. Sensitivity analyses suggested that
under the best-case population-based scenario, SPCs could avert up to 100 million CVD deaths and 250 million non-fatal events,
and reduce premature mortality by 2% (targeted) and 3.2% (population) globally. Although these drugs have not been associated with
increased rates of fatal adverse events, and no rise in event-related mortality was observed, the authors project that widespread use
of Aspirin-containing SPCs from 2023 to 2050 could still result in substantial numbers of non-fatal side effects, including an estimated
150 to 340 million cases of dizziness and approximately 27 million cases of non-fatal gastrointestinal bleeding.
Integrating SPC therapies into clinical practice could yield health gains comparable to complex titration guidelines but with simpler
implementation, particularly in settings with limited primary care capacity. Their widespread use could have an impact on CV
outcomes comparable to achieving the near-elimination of tobacco smoking or reaching an ambitious 80% coverage goal for
hypertension treatment by 2050. The authors stress that SPCs are safe, with mainly mild adverse effects, and should complement,
not replace, lifestyle interventions and existing clinical guidelines. The authors suggest that implementation will require decision
TABLE OF CONTENTS